Walking and Running
Did you know that daily walking and/or running are some of the most important steps in reducing your risk of heart disease, diabetes, osteoporosis and many other serious health conditions?
You may be wanting to improve your well-being, or reduce your risks of health conditions, or simply to start a new hobby, so here are some easy steps to begin your walking/running routine!
- Set realistic targets and goals. This could be a walking/running distance, weight loss (in combination with good diet), or seeing if you can improve your time running around the block.
- Ensure you have the most appropriate shoes possible by seeing a Podiatrist, who can also help you plan your walking/running sessions.
- Start off easy. This could mean a short walk around the block, or a light jog to the milkbar and back. Everyone is different, so do what works for you.
- Set a routine. Put a particular time aside each day for your exercise, and stick to it!
- If you’re feeling lonely, invite your partner, friend, colleague to exercise with you!
- Don’t feel bad if you have to skip a day, just stay positive and look forward to the next session!
- Make sure you’re having fun! Yes, you will get tired and sweaty, but if take notice of your surroundings, play some music and smile, you are on your way to making a beneficial routine!
For further advice on footwear, running, walking, click on the link below to make an appointment or call 1300 847 226.
http://www.thepodiatrygroup.com.au/booking/
Skin Cancer on the Foot?
As Podiatrists we often see moles and spots on people’s feet and toes. Most of the time they’re harmless, however occasionally we come across some that need further investigation.
This isn’t to scare you, but simply to inform you of the importance of checking your feet, even though they may not get exposed to direct sunlight.
It is true that skin cancers can form even where the sun don’t shine!
So what can you do?
- Check your feet every so often for moles and spots.
- Observe for any changes in size, shape or colour.
- Apply sunscreen to your feet when not wearing closed shoes.
- See your GP if you’re worried about a spot, or just want a professional opinion.
Rest assured, if you’re seeing one of us we will make sure to keep an eye on the spots you may have on your feet, and monitor them as we see you into the future.
For further foot advice, visit our website and make an appointment to see one of our friendly Podiatrists!
There are many ways to make a living and for some of us it involves long periods of standing. In particular, jobs that require us to stand all day place an undue stress on our feet, legs, knees, and hips- Did someone say retail worker?
The main problem with standing for long periods of time is that you are placing a large amount of stress on the same muscle groups, ligaments and bones. This is why you can experience pain.
We are all probably a little guilty of fantasizing about quitting our jobs and finally chasing our dream career of becoming a travel show host for Getaway. But we better take a look at a few ways we can reduce pain in the feet, just in case that falls through.
Keeping good foot health while standing will require you to be proactive and take steps towards achieving more cushioning and support during your day to day work.
The last thing anyone wants is an injury that prevents you from working and therefore impacts your income. To the same degree none of us want to work with foot or leg pain either!
To help make it easier, let’s take a moment to answer the question of why my feet hurt from standing all day? And what we can do to help.
Why Do My Feet Hurt From Standing All Day?
People are meant to stand. The reason why it can be challenging and why our feet hurt is that we may not be ready for it without some planning. Many people changing to a more active job will find that pain in their feet occurs pretty quickly after starting. Some of this pain will go away naturally as your body gets accustomed to it. If the pain persists, then it may have something do with your shoes or your foot type.
Sometimes the surfaces that we work on can be a little unforgiving on our joints. Man-made surfaces like concrete and tiles don’t allow for much shock absorption and therefore our joints take all the load. This is where the right pair of shoes can help.
The lifespan of a pair of shoes will change dramatically based on what brand and style of shoe you are wearing. As well as how often you are wearing them and how many kilometres you do in a day.
Wearing the right shoes can dramatically reduce the amount of pain you feel from standing all day. Also, consider how long your shoe is meant to last. As the shoe breaks down from use, it will provide less and less cushion for your body, resulting in experiencing more discomfort.
It is important that you wear the right shoe for your foot type. Just because you spent $200 on a pair of shoes does not necessarily mean they are more supportive or that they are right for you!
The best way to make sure you are getting the right shoe is to book an appointment with one of our shoe addicted podiatrists to have your walking pattern assessed. We can then recommend the right shoe for you before you invest your money into the wrong one!
The bottom line
Don’t put up with unnecessary pain. We are here to help you and will work with you to meet the specific needs of your feet and job.
Call us on 1300 847 226 to make an appointment and give us the time to help you.
We have recently moved into a bigger and better clinic located at Cranbourne Park Health and Wellness Centre, 24 Mundaring Drive, Cranbourne 3977. We are located within short walking distance of Cranbourne Park Shopping Centre and there is ample off-street parking available right in front of our clinic.
With this exciting move, we can offer more open hours and a broad range of services. Our podiatrists can help you with all your footcare needs including:
- Nail and skin care
- Corns and callouses
- Ingrown nails
- Diabetes footcare
- Sports injuries
- Video gait analysis
- Children’s feet
- Moonboots and casting
- EPC Plans
Cranbourne Park Health and Wellness Centre also provides other allied health services including:
- Physiotherapy
- Dietitian
- Psychology
- Audiology
- & more
Our team of professionals are ready to help you from head to toe!
You do not need to have a referral, just call us on 1300 847 226 or book an appointment online.
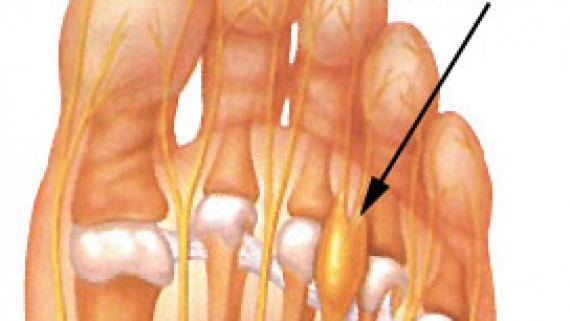
What is a Morton’s neuroma?
How did I get this?
If I had a Morton’s neuroma, what would it feel like?
What do I do next?
- Ice to the area
- Again ladies – avoid high heels!
- Check the width of your footwear. Try wearing wider shoes with a lower heel. Tighter or narrow footwear can compress and bunch the toes together. Your podiatrist can help you with footwear assessment and recommendations.
The exact cause of Morton’s neuroma can be different between patients. An accurate diagnosis can be made by a podiatrist.
- You may require orthotics to alleviate the forefoot pressure and mechanics in combination with metatarsal padding.
- Additional, ultrasound imaging maybe required to consider other diagnostic possibilities (as mentioned in first post).
- In more serve cases a course of anaesthetic and cortisone injections.
- Surgical removal of the neuroma as last resort.
Don’t forget, a neuroma is a result of a nerve that is being traumatised by a poorly functioning foot or footwear and treating the cause of this condition is paramount.
Metatarsalgia – Ball of Foot Pain
So many foot problems can occur in our forefoot. As podiatrists we treat a wide range of problems associated with forefoot pain and deformity. Metatarsalgia is a non-specific term or general umbrella term if you will, for pain in the forefoot or ball of the foot.
Discomfort is usually located beneath the balls of our feet and is typically a result of increased forefoot pressure.
Bunions, hammertoes, short metatarsal bones, stress fractures, plantar plate disruption, Freiberg’s infarction, capsulitis, intermetatarsal bursitis and Morton’s neuroma area some possible causes of metatarsalgia.
Today we are talking about intermetatarsal bursitis.
Intermetatarsal bursitis
What is bursitis?
An inflammation or irritation of the bursa. A bursa is a small fluid-filled sac that provides cushioning and reduces friction, between and around the joints of the forefoot. Irritation of the bursa can cause swelling and pain (bursitis). The intermetatarsal bursae are located on the bottom of the foot near the base of the toes.
Bursitis can also affect other parts of the body – back of the heel/Achilles tendon, the knee, hip, shoulder and elbow.
How did I get this?
Generally, bursitis can occur through injury or repetitive motion causing irritation and inflammation. They can become irritated when one metatarsal bone takes more load than others.
Wearing narrow or excessively worn footwear during the day and different sporting activities can increase your chance of developing bursitis. Other factors can include;
- Overuse or excessive pressure on the forefoot
- Stress from abnormal foot mechanics
- Injury from a fall or hit to the area
- Less commonly due to certain types of arthritis; rheumatoid arthritis, gout, psoriatic arthritis
If I had bursitis, what would it feel like?
Friction can cause the space between the tendon, bone and skin to become inflamed – causing swelling, pain and possibly redness of the surrounding area.
Irritation and restricted movement of the affected joint may be evident and certain footwear or activities may exacerbate pain.
What do I do next?
- Apply ice to the area – this can help reduce inflammation
- Rest and avoid painful activities
- Non-steroidal anti-inflammatories if advised by your pharmacist
- Orthotics
- Footwear changes, avoid high heels!
- Reduce the amount of pressure being place placed on the bursa through off loading
- In chronic cases, injections of local anaesthetic and corticosteroid may be required in combination with padding
It’s important to attend a podiatry consult for assessment to determine the root cause, as other injuries can produce similar symptoms. Podiatrist may advise you on appropriate shoes and can also add padding to off load the pressure, prescribe orthotics and refer for any imaging that may be needed to rule out other conditions.
Contact us on 1300 847 226 or make an appointment online to speak with one of our friendly podiatrists about helping you get back on your feet sooner!
Understanding the need to look after your feet when you have diabetes
What is diabetes?
The pancreas is no longer able to make insulin, or the body cannot make good use of the insulin it does produce.
Insulin enables glucose (sugar), from the food we eat to pass from the blood stream into the cells in the body to make energy.
Not being able to produce insulin or use it effectively can cause raised sugar levels (hyperglycaemia). Over the long-term high sugar levels can damage some tissues and organs in the body.
Type 1 diabetes is usually caused by an auto-immune reaction where the body’s defence system attacks cells that produce insulin. It can occur at any age, however it is more common in children or young adults. Injections of insulin to control sugar levels in the blood is required.
Type 2 diabetes occurs when the body is no longer using insulin efficiently. Sugar builds up in bloodstream and the cells are starved of energy. There may be a family history to developing type 2 diabetes or environmental triggers.
Diabetes and the feet come hand in hand (or foot in foot).
“Every year, more than 4,400 amputations are carried out as a result of diabetes”. (https://www.diabetesaustralia.com.au/national-diabetes-week). Foot complications with diabetes are becoming more prevalent. Prevention through education, understanding foot complications, signs and symptoms and regular assessment is required to prevent hospitalisation and risk of amputation.
Some foot concerns:
- Nerve damage (peripheral neuropathy) and poor circulation in the feet (peripheral arterial disease).
- Loss of feeling, tingling, burning sensation and numbness.
- Poor healing, cramping.
- Increase rate of infection.
- Foot ulcers or sores that may have delayed healing.
- Changes in shape which can cause an increase in pressure .
- Hammer or claw toes, bunions, arthritis.
- Charcot’s arthropathy.
- A rare condition that occurs with good blood flow to the feet and numbness (peripheral neuropathy) – red, hot, swollen foot, rocker bottom foot.
Peripheral neuropathy explained
- Insensitivity or loss of ability to feel; touch, pressure, vibration, pain, heat, cold or perception/position.
- You may not realise you have a cut, blister, corn or footwear rubbing. The damage caused may not heal adequately, which may cause ulceration in some cases.
- Check feet daily for cuts and redness and blisters etc.
Poor circulation explained
- Reduced blood flow and nutrients to the feet
- Swelling and dryness and impaired healing process
- Cold feet
- Painful calves when walking or at night in bed
- Delayed or reduced healing rate in the feet
- Improve – activity, avoid smoking, reduce caffeine
- Control cholesterol and blood sugar levels
Regular podiatry and foot check-ups or assessments are an important part of preventative care for your feet to prevent serious complications. Diabetes assessment every 3-12 months and more regularly treatment for hard skin, corns and nail care is recommended.
Quick and painless tests by your podiatrist include:
- Vascular assessment with an ultrasound testing the amount of blood flow to the feet.
- Neurological assessment testing sensation and your ability to feel.
- Gait (Walking) assessment to assess any increase in pressure due to the change in foot shape.
- Footwear assessment to ensure suitable footwear and fit.
- Skin and nail care to prevent any ingrowing toenails, painful corns and pressure areas.
Preventing foot complications and self-managing tips
- Control your blood sugar levels to reduce the risk of damage to your feet.
- Keeping moving! Blood flow is important for healthy feet.
- Stop smoking – smoking slows down blood flow to the extremities.
- Check feet daily – with a mirror to observe for any cuts or red marks that require attention.
- Good foot hygiene is important. Wash and dry your feet thoroughly daily.
- Be careful with trimming toes nails and avoid cutting down the side.
- Wear comfortable socks and shoes.
- Get fitted professionally for shoes at the end of the day to reduce risk of poorly fitting shoes causing blisters.
- Avoid uncomfortable or tight shoes that rub or cut into your feet.
- Avoid high heels and pointed toes.
- Look inside your shoes daily for any stones, or prominent lining to avoid rubbing against your feet causing blisters.
- Avoid walking barefoot.
- Wear comfortable socks that are a good fit and aren’t too tight.
- Prevent dry skin by applying moisturise daily, avoid cream between the toes.
- See a podiatrist regularly to trim off callous, remove corns and trim toenails.
- Podiatry diabetes assessment.
In summary…
Of course not all foot problems will require a hospital visit, but they can vary from minor complications to wounds that won’t heal. Serious complications can be avoided through self-management and through regular check-ups.
Simple injuries such as corns, cuts, or callouses, when combined with loss of sensation in the feet can mean that these injuries go unnoticed. If untreated they may not heal due to lack of blood supply and infection can occur. Foot assessment by a podiatrist is recommended to establish your foot health status by determining the blood flow and sensation in your feet and identify any potential risk areas.
- Look at your feet daily.
Melbourne Marathon Podiatry Tips
At The Podiatry Group we are often asked for our top tips when training for a marathon. With the Melbourne Marathon coming up we have decided to give you a little insight to some helpful guidelines to consider when training and running in a marathon. The internet can provide a whole text book of information from how to carb load before an event to the best anti chafing stick to use. We will let you in on the best advice we provide for runner’s feet during their marathon.
- Get your runners professionally fitted. There are stores like Active Feet who are highly trained to fit running shoes. They can observe your running and walking patterns on a treadmill to better assess which shoe is most appropriate for you. Remember that runners will only last on average between 600-800kms so if you have been training hard make sure that by the time you reach your marathon day, your shoes still have life in them. If you are considering purchasing a new pair of shoes before your marathon, make sure that you have enough time to wear them in slowly before the big day. This means that you should have them at least 2 weeks before your event and begin wearing them in at home for a few hours and gradually progressing to a walk then a run. If you are purchasing the same brand and style as your last shoe make sure you speak with the person selling you your shoes to see if there have been any significant changes between the last and latest model. Sometimes the heel height (heel pitch) of a shoe will reduce or increase compared to the forefoot. This may alter the way that you run and impact the style of running you have trained for. At The Podiatry Group we are able to help assess your runners and ensure they are the right shoe for your running style and technique.
- Make sure you have the right socks. This may seem a silly statement; some of you may think that all socks are equal. We are here to tell you that they are not. There are socks that are designed to help prevent blistering. A small blister might not seem too daunting, but over a 42km run it can slowly but surely cause you more discomfort then you could imagine. There are socks that are specifically designed to wick moisture away from the feet leaving them dry. Some brands that are able to do this are Thorlo, Wigwam and Injinji.
- Make sure your nails are cut! Cut your nails before an event but leave 1mm of nail growth at the end (1mm of the white part of the nail), this will ensure you don’t cut the too short and bleed causing a bit of a mess and some sore toes before you even begin running. This will also help minimise the risk of your nails going black from bruising or even losing your nails after a marathon. Sometimes our nails get blackened or fall off after an event like a marathon from repetitive micro-trauma. This can be where our toes hit the end of our shoes when running causing micro damage to the nail. This can also be due to our shoes not being laced properly.
- Get rid of that build up of hard skin! If you have callous on your feet then odds are you have a lot of pressure and friction occurring at that site. If you would like this professionally removed then contact us. If you only have a small amount and think you can manage yourself then the best way is to use a pumice stone. A pumice stone must be used wet (in the bath or shower), it is best used if you rub the pumice stone on a cake of soap and then on the hardened skin until you have taken enough off.
- Compression stockings can help aid recovery time. It has been shown that an average persons calf will expand in diameter after standing for 1-3 hours. As such, you can imagine that when running a marathon (which could take anywhere between 3-5 hours depending on your speed) your calf will expand and could cause discomfort and a feeling of fatigue. We recommend that all runners consider compression stockings. Please note that we strongly advise that a runner come in for an assessment before using a high grade compression stocking.
- Have fun! You may choose to run a marathon only once in your life or you may be crazy enough to run many times. Our most important tip we could give you is to enjoy it. You’ve worked so hard to get to where you are, all those training sessions, all that blood sweat and tears, just don’t forget to enjoy yourself.
If you are training for a marathon and want to speak with one of our Podiatrists then you can contact us. We have Podiatry Clinics located in Cranbourne, Drouin and Warragul.
Sore Feet at the races
With Spring Carnival Racing just around the corner we have decided to let you in on our closest secrets to keeping your feet looking and more importantly feeling fabulous at the races. Don’t put up with sore feet anymore.
Women all over Victoria will be flooding the shops looking for fabulous fascinators, cute clutches and horrendously high heels. We will give you the inside scoop on what to look for when it comes to footwear at the races and how to prevent those dreaded sore feet. We understand the perils of looking good at the races, a little bit of discomfort is expected but we want to make sure you aren’t hobbling home on feet filled with blisters, swelling and bruising.
After a day in those beautiful strappy heels you can be faced with a very difficult decision; To walk home crippled, feeling intense pain and burning with every step or to take the shoes off and face the risk of contracting something terrible from the sticky alcohol smeared ground?
We offer you a new option! Be prepared and follow our tips to be leaving the races with your head held high, your footwear on and hopefully with a pocket full of cash from all of your winning horses.
What shoes should I wear?
When it comes to picking a shoe that you will be spending all day walking and standing in it is important to take comfort into account. After all, we can’t spend all day sitting around, ordering our friends to place our bets, serve us drinks and shade us from the sun! To avoid sore feet don’t pick the highest stiletto with as many straps to rival a salsa dancer. Think a little more conservatively. A wider heel helps distribute force over a larger area, meaning less pain. You could also look for a heel that has a platform at the front of the shoe. This way you can look like your wearing 6 inch heels without your toes constantly slipping to the front of your shoe.
A wedge is also a great shoe to consider for Spring Racing, No one ever sunk into soft grass in a wedge! (Our motto is “No woman left behind!”) If you pick a shoe that is a similar shape to your foot you will be amazed with the comfort this will offer. Some shoes have really pointy ends and will cause your toes to be squished. Although this may look great they are better saved for a dinner date where you can be sitting most of the time.
Another consideration to make is how is your foot going to stay inside your shoe? This may seem a silly question to ask but as women, we know all to well that in certain footwear our heels can slip out of the back. This may be okay the first few times but after the 499th time it can get a little old- Not to mention cause enough friction to start a fire at the back of our heel! A strap at the front of the shoe will ensure our foot stays in place. Less movement of our foot inside the shoes means less friction and therefore less likelihood of blisters. You will also spend less time clawing at your shoes to keep them on when walking- you would be surprised with how tiring this can be.
When it comes to picking what material the shoe is made out of, natural is always best. Leather is a great material that will mould to the shape of your foot with repeated wear. This means that if you “break in your shoes” properly before the big day you will have already altered the shape of the outside of the shoe to help it fit better. We always recommend to wear your shoes for a few hours at a time in the weeks leading up to a big event. It’s like a marathon- if you don’t put in the training ladies you will regret it on the day! The only leather we advise to be cautious with it patent leather. The name may be a little misleading, it doesn’t have the same feel as leather as it has been coated which makes it stiff and unforgiving. This means it will not mould well to your feet and will be about as sore on the day as when you are breaking them in.
Stockings are a great option to consider too! They help prevent your feet from rubbing inside the shoe. They come in a range of colours to match your natural skin colour and they can even prevent you from having to fake tan. The stocking has evolved from what we remember our grandmas wearing when we were young. They even have the peep toe variety so you can wear them in open toe shoes and not have to worry about a seam showing. Stockings also apply pressure around our legs and ankles; this can help stop swelling when we have spent all day standing. Something that will be greatly appreciated at the end of the day.
The Podiatry Group have sourced some great looking and comfortable footwear brands that you can be confident will provide you with the support and comfort needed to face a day at the Spring Races.
Bared Footwear is a great brand that has many heels, wedges and flats with arch support built in. The reason these are so fabulous and comfortable is that a female Melbourne podiatrist has designed them and understands exactly the fine line between fashion and comfort.
Ziera is another brand that provide great quality shoes with built in arch supports.
Visiting your podiatrist before the races is a great way to ensure your feet are looking fabulous and fresh. You don’t want cracked heels or discoloured nails stopping you from wearing open shoes. That’s where we can help. Come visit our Podiatrists at Cranbourne, Drouin or Warragul.
Remember to keep all the above tips in mind when considering your footwear at the races.
From the friendly team at TPG.