- Strict waiting room limits apply – we ask that ALL patient now call us from the car park on arrival, stay in your car, and we will return your call when it’s time to come inside
- Sanitisation stations remain in the clinic, and their use is a condition of entry to the practice
- Podiatrists will continue to be wearing masks, gloves and gowns during appointment times
And finally, once again, it is important to continue to follow the rules for testing and/or isolation should you have come into contact with someone confirmed or suspected of carrying the virus, or are suffering any upper respiratory symptoms. If you are unwell, please reschedule your appointment and we’ll look forward to seeing you back in the clinic once you’re able.
We ask that you take special caution when returning from overseas travel to high-risk areas and ask that you contact us to reschedule your appointment if you suffer cold/flu-like symptoms or have visited a high-risk country within the last 14 days.
If you need to contact us or have any queries or concerns please feel free to phone our clinic on 1300 847 226.
We’d like to take this opportunity to thank you for your support and your trust in us for all your podiatry care.
The Podiatry Group
Walking and Running
Did you know that daily walking and/or running are some of the most important steps in reducing your risk of heart disease, diabetes, osteoporosis and many other serious health conditions?
You may be wanting to improve your well-being, or reduce your risks of health conditions, or simply to start a new hobby, so here are some easy steps to begin your walking/running routine!
- Set realistic targets and goals. This could be a walking/running distance, weight loss (in combination with good diet), or seeing if you can improve your time running around the block.
- Ensure you have the most appropriate shoes possible by seeing a Podiatrist, who can also help you plan your walking/running sessions.
- Start off easy. This could mean a short walk around the block, or a light jog to the milkbar and back. Everyone is different, so do what works for you.
- Set a routine. Put a particular time aside each day for your exercise, and stick to it!
- If you’re feeling lonely, invite your partner, friend, colleague to exercise with you!
- Don’t feel bad if you have to skip a day, just stay positive and look forward to the next session!
- Make sure you’re having fun! Yes, you will get tired and sweaty, but if take notice of your surroundings, play some music and smile, you are on your way to making a beneficial routine!
For further advice on footwear, running, walking, click on the link below to make an appointment or call 1300 847 226.
http://www.thepodiatrygroup.com.au/booking/
Skin Cancer on the Foot?
As Podiatrists we often see moles and spots on people’s feet and toes. Most of the time they’re harmless, however occasionally we come across some that need further investigation.
This isn’t to scare you, but simply to inform you of the importance of checking your feet, even though they may not get exposed to direct sunlight.
It is true that skin cancers can form even where the sun don’t shine!
So what can you do?
- Check your feet every so often for moles and spots.
- Observe for any changes in size, shape or colour.
- Apply sunscreen to your feet when not wearing closed shoes.
- See your GP if you’re worried about a spot, or just want a professional opinion.
Rest assured, if you’re seeing one of us we will make sure to keep an eye on the spots you may have on your feet, and monitor them as we see you into the future.
For further foot advice, visit our website and make an appointment to see one of our friendly Podiatrists!
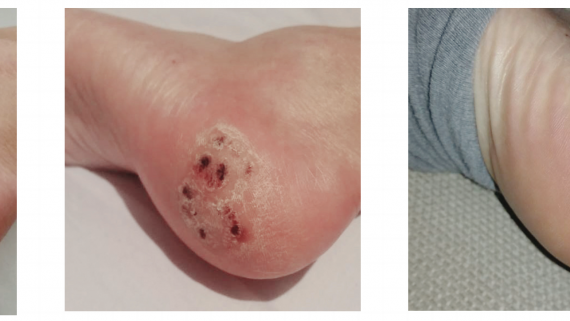
Finally a quick and effective solution for Warts!
What is Swift?
Swift was developed in the UK for the treatment of warts. It has since become a phenomenon due to it’s ease of use and success in ridding patients of unwanted warts. It is now available in Australia and we are happy to say you can receive this treatment at our clinics.
Swift uses microwave energy, which is delivered through a special probe applied to the skin to treat the affected tissue. Multiple verrucas/warts can be treated at a single session. The treatment is quick, efficient with minimal pain. No anaesthetic or dressings are needed.
Does it hurt?
Like many treatments for skin lesions, some minor discomfort may be experienced.
Pain levels vary from person to person but most people undergoing swift microwave therapy liken it to to a sudden heat, lasting 2 – 3 seconds then quickly subsiding.
What can I do after treatment?
In some cases the treated area may feel sore, but it will not prevent you undertaking normal daily activities. No dressings are needed and you can get your foot wet.
How many treatments will I need?
This is dependent on how you respond to treatment. In some cases, you may need more than one treatment. Your podiatrist will be able to discuss this with you.
In recent research, 83% of the most stubborn warts cleared using Swift Microwave Therapy. The very best results were obtained with 3 treatments at 4 weekly intervals.
Can anyone receive this treatment?
With a few exceptions, most people with skin lesions would be able to have this treatment. It is suitable for children and diabetics who have good circulation. Your podiatrist will carry out an assessment prior to treatment and be able to advise you on this.
Happy to help.
Give us a call on 1300 847 226 and chat to us about starting your Swift Therapy today. We have clinics located in Warragul, Drouin and Cranbourne.
You can also jump on our website and book online.
There are many ways to make a living and for some of us it involves long periods of standing. In particular, jobs that require us to stand all day place an undue stress on our feet, legs, knees, and hips- Did someone say retail worker?
The main problem with standing for long periods of time is that you are placing a large amount of stress on the same muscle groups, ligaments and bones. This is why you can experience pain.
We are all probably a little guilty of fantasizing about quitting our jobs and finally chasing our dream career of becoming a travel show host for Getaway. But we better take a look at a few ways we can reduce pain in the feet, just in case that falls through.
Keeping good foot health while standing will require you to be proactive and take steps towards achieving more cushioning and support during your day to day work.
The last thing anyone wants is an injury that prevents you from working and therefore impacts your income. To the same degree none of us want to work with foot or leg pain either!
To help make it easier, let’s take a moment to answer the question of why my feet hurt from standing all day? And what we can do to help.
Why Do My Feet Hurt From Standing All Day?
People are meant to stand. The reason why it can be challenging and why our feet hurt is that we may not be ready for it without some planning. Many people changing to a more active job will find that pain in their feet occurs pretty quickly after starting. Some of this pain will go away naturally as your body gets accustomed to it. If the pain persists, then it may have something do with your shoes or your foot type.
Sometimes the surfaces that we work on can be a little unforgiving on our joints. Man-made surfaces like concrete and tiles don’t allow for much shock absorption and therefore our joints take all the load. This is where the right pair of shoes can help.
The lifespan of a pair of shoes will change dramatically based on what brand and style of shoe you are wearing. As well as how often you are wearing them and how many kilometres you do in a day.
Wearing the right shoes can dramatically reduce the amount of pain you feel from standing all day. Also, consider how long your shoe is meant to last. As the shoe breaks down from use, it will provide less and less cushion for your body, resulting in experiencing more discomfort.
It is important that you wear the right shoe for your foot type. Just because you spent $200 on a pair of shoes does not necessarily mean they are more supportive or that they are right for you!
The best way to make sure you are getting the right shoe is to book an appointment with one of our shoe addicted podiatrists to have your walking pattern assessed. We can then recommend the right shoe for you before you invest your money into the wrong one!
The bottom line
Don’t put up with unnecessary pain. We are here to help you and will work with you to meet the specific needs of your feet and job.
Call us on 1300 847 226 to make an appointment and give us the time to help you.
Ankle sprains are one of the most common leg injuries that podiatrists treat every day. You can twist an ankle during sport, at work or just minding your own business at home. Whether you have twisted an ankle for the first time or the 10th time, it is a good idea to book an appointment with your podiatrist.
We can help you from start to finish. From a thorough assessment of the damage to the ankle to getting you back on your feet and doing what you love best.
Assessment of ankle sprains is very important, as there may be very little damage to the structures in the ankle or there can be a complicated bone fracture requiring urgent attention. For this reason, your podiatrist may need to refer you for ultrasound or x-ray imaging. Depending on the severity, we may cast the ankle or fit you with a moonboot. If the sprain is minor, a good supportive pair of runners may be recommended.
Once an ankle sprain is healed, a rehabilitation program is key to getting back to your activities and preventing ankle injuries in the future. Your podiatrist will develop a customised strengthening program to improve your balance and ankle strength and monitor your progress on a regular basis.
Don’t let that ankle sprain keep you down, book an appointment with The Podiatry Group on 1300 847 226.
As the clouds (eventually) start to clear we are reminded that Spring is upon us. It’s time to dust off those runners, get outside and start enjoying a bit of sunshine. If your runners are looking a little bit too dusty or your feet are feeling sore or fatigued when wearing them, it may be time for an update.
At The Podiatry Group, we can perform a biomechanical assessment of your feet. We look at your foot posture and your gait (the way you walk) to determine which type of runner would suit you best. Many people aren’t aware that runners should be replaced every 6-12 months if you have a relatively active lifestyle. The reason for this is that the structure of the shoe wears away over time and use, and the foam of the shoe compresses. A new pair of runners is often all you need to get that spring back in your step.
If you have got supportive footwear already but do find your feet and legs feel sore or fatigued, our assessment can help determine other factors that might be contributing to your pain. We can look at your activity levels and training/work surfaces to build an exercise plan that works for you.
Our management plan may also include a stretching and strengthening plan, activity modification, foot orthotics and ongoing regular assessments to make sure everything is running smoothly- the same way we want you to run!
Book and appointment with us online or call us on 1300 847 226.
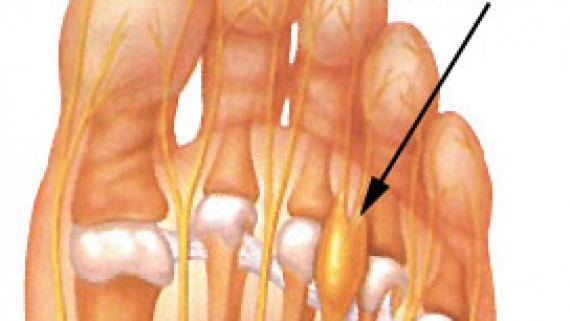
What is a Morton’s neuroma?
How did I get this?
If I had a Morton’s neuroma, what would it feel like?
What do I do next?
- Ice to the area
- Again ladies – avoid high heels!
- Check the width of your footwear. Try wearing wider shoes with a lower heel. Tighter or narrow footwear can compress and bunch the toes together. Your podiatrist can help you with footwear assessment and recommendations.
The exact cause of Morton’s neuroma can be different between patients. An accurate diagnosis can be made by a podiatrist.
- You may require orthotics to alleviate the forefoot pressure and mechanics in combination with metatarsal padding.
- Additional, ultrasound imaging maybe required to consider other diagnostic possibilities (as mentioned in first post).
- In more serve cases a course of anaesthetic and cortisone injections.
- Surgical removal of the neuroma as last resort.
Don’t forget, a neuroma is a result of a nerve that is being traumatised by a poorly functioning foot or footwear and treating the cause of this condition is paramount.
Metatarsalgia – Ball of Foot Pain
So many foot problems can occur in our forefoot. As podiatrists we treat a wide range of problems associated with forefoot pain and deformity. Metatarsalgia is a non-specific term or general umbrella term if you will, for pain in the forefoot or ball of the foot.
Discomfort is usually located beneath the balls of our feet and is typically a result of increased forefoot pressure.
Bunions, hammertoes, short metatarsal bones, stress fractures, plantar plate disruption, Freiberg’s infarction, capsulitis, intermetatarsal bursitis and Morton’s neuroma area some possible causes of metatarsalgia.
Today we are talking about intermetatarsal bursitis.
Intermetatarsal bursitis
What is bursitis?
An inflammation or irritation of the bursa. A bursa is a small fluid-filled sac that provides cushioning and reduces friction, between and around the joints of the forefoot. Irritation of the bursa can cause swelling and pain (bursitis). The intermetatarsal bursae are located on the bottom of the foot near the base of the toes.
Bursitis can also affect other parts of the body – back of the heel/Achilles tendon, the knee, hip, shoulder and elbow.
How did I get this?
Generally, bursitis can occur through injury or repetitive motion causing irritation and inflammation. They can become irritated when one metatarsal bone takes more load than others.
Wearing narrow or excessively worn footwear during the day and different sporting activities can increase your chance of developing bursitis. Other factors can include;
- Overuse or excessive pressure on the forefoot
- Stress from abnormal foot mechanics
- Injury from a fall or hit to the area
- Less commonly due to certain types of arthritis; rheumatoid arthritis, gout, psoriatic arthritis
If I had bursitis, what would it feel like?
Friction can cause the space between the tendon, bone and skin to become inflamed – causing swelling, pain and possibly redness of the surrounding area.
Irritation and restricted movement of the affected joint may be evident and certain footwear or activities may exacerbate pain.
What do I do next?
- Apply ice to the area – this can help reduce inflammation
- Rest and avoid painful activities
- Non-steroidal anti-inflammatories if advised by your pharmacist
- Orthotics
- Footwear changes, avoid high heels!
- Reduce the amount of pressure being place placed on the bursa through off loading
- In chronic cases, injections of local anaesthetic and corticosteroid may be required in combination with padding
It’s important to attend a podiatry consult for assessment to determine the root cause, as other injuries can produce similar symptoms. Podiatrist may advise you on appropriate shoes and can also add padding to off load the pressure, prescribe orthotics and refer for any imaging that may be needed to rule out other conditions.
Contact us on 1300 847 226 or make an appointment online to speak with one of our friendly podiatrists about helping you get back on your feet sooner!
The battle of the fungal nail!
Fungal toenails or onychomycosis is common, unpleasant and persistent in nature. Accounting for almost half of all nail problems, this slow growing infection occurs when microscopic fungi gain entry to the nail, usually through small trauma. Trauma allows the pathogen to enter the nail and nail bed.
Other causes
- Fungal organisms grow and spread in warm, moist environments and are usually picked up in warm damp areas like socks, shoes, public pools, gyms and showers.
- Not drying off the feet thoroughly following showers or exercise and wearing tight shoes or socks, can provide conditions the fungus needs for growth.
- People who have a compromised immune system, diabetes, circulatory problems and the elderly are particularly susceptible.
Symptoms
Fungal nail infections are contagious and can often spread from skin to nails. The poor cosmetic appearance that usually develops can cause some embarrassment. Nails can become discoloured, thickened, brittle, rough and weaken. Sometimes the infection can occur with an odour and can cause discomfort.
Types of Onychomycosis
Distal subungual onychomycosis – most common form of fungal nail that can cause the nail to become yellow brownish in colour, thickened, rough or crumbling.
Superficial white onychomycosis – this type of infection occurs on the outer surface and often appears as white spots. It is the easiest type of infection to treat.
Proximal subungual onychomycosis – occurs in the area of new nail growth at the beginning of the nail and is the least common.
Candida onychomycosis – typically occurs after trauma or damage to the nail that allows the fungus to invade. Most often occurs in people who frequently have their feet in water.
Treatment
As many people with fungal toenails can appreciate, it’s often difficult to eradicate fungal toenail infections, and like most things, prevention is always better than cure. Treatment varies depending on the type of fungal nail infection and the amount of nail involved, so it’s best to chat to your podiatrist who can recommend the best treatment option for your type of onychomycosis. In many cases nail lacquer medications are used, and in severe cases oral antifungal medication from your doctor, however this comes with potential side-effects.
Preventative measures
- Wear protective shoes in public showers and pool areas.
- Wash your feet regularly and dry them thoroughly when they get wet.
- Change socks daily, more regularly if you have increase perspiration or exercise.
- Avoid leaving toenail polish in place for long periods of time, wearing nail polish is not advised for those people who are suffering from nail fungus as it may encourage it to grow.
- Avoid nail solons who re-use their nail instruments, all instruments should be sterilised using an autoclave.
- Wear properly fitting shoes
If you suspect a toenail fungus, it’s recommended you see your podiatrist before it spreads. Podiatrists also have a tool to reduce thickness of fungal nails, this can enable topical medication to absorb and penetrate the nail easier, provide comfort of thickened nails and can help improve the appearance of the nail.
If you or someone you know would benefit from fungal nail treatment, please give us a call or book an appointment online at any of our podiatry clinics in Warragul, Drouin, Beaconsfield or Cranbourne.