Walking and Running
Did you know that daily walking and/or running are some of the most important steps in reducing your risk of heart disease, diabetes, osteoporosis and many other serious health conditions?
You may be wanting to improve your well-being, or reduce your risks of health conditions, or simply to start a new hobby, so here are some easy steps to begin your walking/running routine!
- Set realistic targets and goals. This could be a walking/running distance, weight loss (in combination with good diet), or seeing if you can improve your time running around the block.
- Ensure you have the most appropriate shoes possible by seeing a Podiatrist, who can also help you plan your walking/running sessions.
- Start off easy. This could mean a short walk around the block, or a light jog to the milkbar and back. Everyone is different, so do what works for you.
- Set a routine. Put a particular time aside each day for your exercise, and stick to it!
- If you’re feeling lonely, invite your partner, friend, colleague to exercise with you!
- Don’t feel bad if you have to skip a day, just stay positive and look forward to the next session!
- Make sure you’re having fun! Yes, you will get tired and sweaty, but if take notice of your surroundings, play some music and smile, you are on your way to making a beneficial routine!
For further advice on footwear, running, walking, click on the link below to make an appointment or call 1300 847 226.
http://www.thepodiatrygroup.com.au/booking/
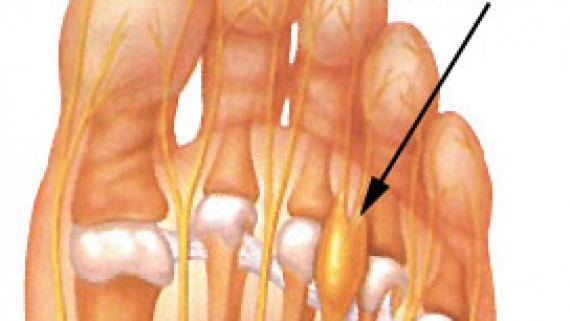
What is a Morton’s neuroma?
How did I get this?
If I had a Morton’s neuroma, what would it feel like?
What do I do next?
- Ice to the area
- Again ladies – avoid high heels!
- Check the width of your footwear. Try wearing wider shoes with a lower heel. Tighter or narrow footwear can compress and bunch the toes together. Your podiatrist can help you with footwear assessment and recommendations.
The exact cause of Morton’s neuroma can be different between patients. An accurate diagnosis can be made by a podiatrist.
- You may require orthotics to alleviate the forefoot pressure and mechanics in combination with metatarsal padding.
- Additional, ultrasound imaging maybe required to consider other diagnostic possibilities (as mentioned in first post).
- In more serve cases a course of anaesthetic and cortisone injections.
- Surgical removal of the neuroma as last resort.
Don’t forget, a neuroma is a result of a nerve that is being traumatised by a poorly functioning foot or footwear and treating the cause of this condition is paramount.
Metatarsalgia – Ball of Foot Pain
So many foot problems can occur in our forefoot. As podiatrists we treat a wide range of problems associated with forefoot pain and deformity. Metatarsalgia is a non-specific term or general umbrella term if you will, for pain in the forefoot or ball of the foot.
Discomfort is usually located beneath the balls of our feet and is typically a result of increased forefoot pressure.
Bunions, hammertoes, short metatarsal bones, stress fractures, plantar plate disruption, Freiberg’s infarction, capsulitis, intermetatarsal bursitis and Morton’s neuroma area some possible causes of metatarsalgia.
Today we are talking about intermetatarsal bursitis.
Intermetatarsal bursitis
What is bursitis?
An inflammation or irritation of the bursa. A bursa is a small fluid-filled sac that provides cushioning and reduces friction, between and around the joints of the forefoot. Irritation of the bursa can cause swelling and pain (bursitis). The intermetatarsal bursae are located on the bottom of the foot near the base of the toes.
Bursitis can also affect other parts of the body – back of the heel/Achilles tendon, the knee, hip, shoulder and elbow.
How did I get this?
Generally, bursitis can occur through injury or repetitive motion causing irritation and inflammation. They can become irritated when one metatarsal bone takes more load than others.
Wearing narrow or excessively worn footwear during the day and different sporting activities can increase your chance of developing bursitis. Other factors can include;
- Overuse or excessive pressure on the forefoot
- Stress from abnormal foot mechanics
- Injury from a fall or hit to the area
- Less commonly due to certain types of arthritis; rheumatoid arthritis, gout, psoriatic arthritis
If I had bursitis, what would it feel like?
Friction can cause the space between the tendon, bone and skin to become inflamed – causing swelling, pain and possibly redness of the surrounding area.
Irritation and restricted movement of the affected joint may be evident and certain footwear or activities may exacerbate pain.
What do I do next?
- Apply ice to the area – this can help reduce inflammation
- Rest and avoid painful activities
- Non-steroidal anti-inflammatories if advised by your pharmacist
- Orthotics
- Footwear changes, avoid high heels!
- Reduce the amount of pressure being place placed on the bursa through off loading
- In chronic cases, injections of local anaesthetic and corticosteroid may be required in combination with padding
It’s important to attend a podiatry consult for assessment to determine the root cause, as other injuries can produce similar symptoms. Podiatrist may advise you on appropriate shoes and can also add padding to off load the pressure, prescribe orthotics and refer for any imaging that may be needed to rule out other conditions.
Contact us on 1300 847 226 or make an appointment online to speak with one of our friendly podiatrists about helping you get back on your feet sooner!
Online Bookings
Online bookings are now available at The Podiatry Group.
For your convenience we have online bookings available across our Warragul, Drouin and Cranbourne clinics.
Your step towards better foot health is just one click away. Click here to book now.